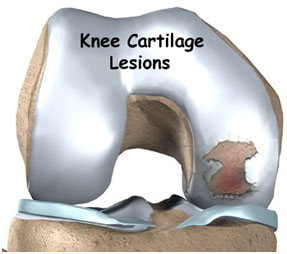
Cartilage, most notably the cartilage surface that which is found in the knee joint, is generally characterized by very low friction, high wear resistance, and poor regenerative qualities. It is responsible for much of the compressive resistance and load bearing qualities of the knee joint and, without it, walking is painful to impossible.
Osteoarthritis is a common condition of cartilage failure that can lead to limited range of motion, bone damage and invariably, pain. Due to a combination of acute stress and chronic fatigue, osteoarthritis directly manifests itself in a wearing away of the articular surface and, in extreme cases, bone can be exposed in the joint.
Some additional examples of cartilage failure mechanisms include cellular matrix linkage rupture, chondrocyte protein synthesis inhibition, and chondrocyte apoptosis. There are several different repair options available for cartilage damage or failure.
A recent review of more than 30,000 knee arthroscopies by Curl revealed that more than 60% of patients had evidence of Grade III or IV
chondral lesions. When broken down by location:
- 48% of patients had an defect in the medial compartment of the knee,
- 45% in the patellofemoral compartment, and
- 25% in the lateral compartment.
Articular cartilage has limited potential to heal, and defects left untreated often result in continued pain, limited mobility, and progressive degenerative changes.
Although a variety of surgical treatment options are
available, a variety of factors – including lesion size, location, degree of bone loss, and presence of multiple lesions – play an important role in formulating the optimal treatment plan for these injuries.